Wet brain, also known as Wernicke-Korsakoff syndrome (WKS), is a brain disorder caused by excessive alcohol consumption. It can lead to memory loss, confusion, and fatigue - and there’s currently no cure. This condition is difficult for patients and loved ones, but there are a few ways to reduce side effects and get medical help before it becomes permanent.
Read everything you need to know about wet brain syndrome, including its causes, symptoms, possible treatment options, and risk factors.
Whether you're looking for the latest vitamins and supplements, want to stock up on over the counter medication, or are looking for a digital solution for your regular prescription, our providers have you covered. Compare brands below and click on your favourite to shop their best offers now!
What is wet brain?
Wet brain is a brain disorder that develops if you have a severe thiamin deficiency. Also known as vitamin B1, you need this essential vitamin to aid your body’s nerve, brain, muscle, and heart functions. In addition, many key enzymes in the brain need thiamin to function properly. This includes important neurotransmitters, meaning you can experience permanent brain damage if you don’t get enough vitamin B1 over a long period.
Wet brain syndrome is a serious condition. It can affect your long-term memory and learning abilities, prompting symptoms similar to Alzheimer’s disease or dementia. This illness is often mistaken for alcohol use disorder as the symptoms of wet brain are very similar to intoxication, such as confusion and abnormal muscle movements. This makes it hard to spot wet brain if you’re also a heavy drinker.
A healthcare professional will check for signs of alcohol use disorder when diagnosing wet brain, and they’ll also check your thiamine levels and give you an MRI to see if you need to follow any further treatment options.
The stages of wet brain
Wet brain develops in two stages: Wernicke's encephalopathy and Korsakoff's psychosis. Named after neurologist Carl Wernicke and neuropsychiatrist Sergei Korsakoff, it’s important to understand how these different stages can affect symptoms, diagnosis, and treatment.
Wernicke's encephalopathy
This is the first stage of wet brain. It’s a temporary condition that can be reversed with the proper treatment. However, Werenicke’s encephalopathy is commonly misdiagnosed or ignored, so it’s important to seek immediate medical advice if you spot any signs of this brain disorder in yourself or a patient in your care.
Short-term symptoms of Wernicke’s encephalopathy may include:
- Difficulty with simple daily tasks like getting dressed.
- Confusion.
- Vision changes.
- Loss of muscle coordination, such as problems standing.
If you take thiamine supplements at this stage of wet brain, you may be able to stop Wernicke’s encephalopathy from developing into the second, more severe stage of wet brain, Korsakoff’s psychosis. However, unfortunately, the majority of people with alcohol use disorder who get Wernicke’s encephalopathy eventually see it grow into Korsakoff’s psychosis.
If you or someone you know is diagnosed with Wernicke’s encephalopathy, ensure you take any prescribed vitamin B1 supplements and alter your lifestyle habits to stop this syndrome from developing into Korsakoff’s psychosis.
Korsakoff's psychosis
The second stage of wet brain is chronic and irreversible, leading to memory impairment and muscle coordination issues. Also known as alcoholic dementia, people with Korsakoff’s psychosis may find it hard to form new memories.
Korsakoff’s psychosis harms the brain regions that regulate short-term memory. This condition also damages the thalamus and hypothalamus, which are responsible for managing various aspects of your health, including your motor skills. As a result, people with wet brain often find it difficult to control their movements.
What causes wet brain?
Although alcohol addiction is the main cause of wet brain syndrome, there are a few other risk factors associated with this brain disorder. Let’s take a look at the different causes of wet brain.
Alcohol abuse and wet brain
According to the National Institute on Alcohol Abuse and Alcoholism, 80% of people with alcohol use disorder also suffer from a thiamine deficiency, which can lead to permanent brain damage. This is because alcohol abuse affects the absorption of thiamine from the intestine, reducing your levels of stored thiamine in the liver. Over time, a lack of thiamine can cause a deficiency in vitamin B1, leading to brain damage and the development of wet brain.
The effects of alcohol can also lead to other health problems, such as kidney failure, heart problems, liver disease, mental health concerns, and nervous system damage - and some of these issues are additional risk factors for wet brain disorder, too.
Other risk factors for wet brain
A few other risk factors can affect your body’s ability to get enough thiamine, leading to wet brain disorder. These factors include:
- HIV or AIDS.
- Kidney failure.
- Liver disease.
- Thyrotoxicosis - this causes high thyroid levels.
- Heart failure treated with diuretic therapy.
- Eating disorders such as anorexia nervosa.
If you’re in the advanced stages of cancer or experience severe nausea and vomiting, you may also develop a thiamine deficiency over a long period. Speak to a healthcare professional for advice and support if you have any of these health conditions to ensure you stay on top of your vitamin B1 intake.
You may also experience the first stage of wet brain, Wernicke’s encephalopathy, if you struggle with malnutrition. Fortunately, this stage is reversible with the right changes by a healthcare provider, as long as you get your diagnosis as early as possible.
Symptoms of wet brain
Wet brain syndrome has many common symptoms, including those of Korsakoff's psychosis and Wernicke's encephalopathy.
The most common signs of wet brain include:
- Memory problems, such as memory loss and the inability to form new memories.
- Muscle coordination issues, such as trouble standing and walking.
- Double vision.
- Abnormal eye movements, such as drooping eyelids.
- Drowsiness and fatigue.
- Trouble with focus and attention.
- Visual or auditory hallucinations.
Confabulation is also a common sign of wet brain, particularly Korsakoff’s psychosis. This specific neuropsychiatric disorder causes you to create a false memory, without intending to trick or deceive someone. As the characteristics of wet brain are very similar to those you may experience when intoxicated, it’s essential to look out for these signs when sober.
How to treat wet brain
Unfortunately, there’s no cure for wet brain. However, if you’re diagnosed with Wernicke’s encephalopathy, you may be able to reverse your symptoms using certain treatment options, but this is only effective if you catch it early enough.
Read about the different coping mechanisms and potential treatment options for wet brain, including addiction management and key dietary changes to follow.
Treating early diagnosis
There are a few ways to manage your early diagnosis of Wernicke’s encephalopathy. Your doctor may prescribe high-dose thiamin supplements to encourage your body to absorb more of this essential vitamin. These supplements are available to take orally or intravenously.
As a poor diet can lead to wet brain, introducing a balanced diet can help to increase your thiamine levels and improve your overall health and well-being. Your healthcare professional will advise you about introducing more vitamin B1 naturally into your diet, too.
Thiamin-rich foods include:
- Fortified cereals.
- Fish.
- Beans and lentils.
- Sunflower seeds.
- Peas.
You’ll need to stop drinking while you receive treatment for this condition. Ideally, you should also stop drinking after you recover from Wernicke’s encephalopathy, or your symptoms may return. Make sure to speak to a doctor to avoid any damaging withdrawal symptoms.
Managing Korsakoff’s psychosis
There are no known treatment options for this long-term stage of wet brain. However, a few helpful coping mechanisms can improve the quality of life for someone dealing with wet brain.
If you’re supporting a family member, try to break down difficult tasks into smaller steps that are easier to follow. You can also arrange a loved one’s home so that essential items are easy to find, and ensure they have a structured routine to minimize stress and confusion.
It’s also important to give your relative independence. Instead of doing a task for them, try showing them how to do it themselves.
Treating alcohol addiction
As alcohol consumption is one of the main causes of wet brain syndrome, treating your addiction can help you prevent this condition or reverse its symptoms in the early stages.
Your doctor may offer various addiction treatments to help you manage alcohol use disorder if this is at the root of your thiamine deficiency. For example, you may need to go through a medically supervised detox to help you stop drinking in safety, especially if you’re at risk of harmful alcohol withdrawal side effects.
You may also need to follow an addiction treatment program. This can include options such as:
- Therapy or counseling.
- Self-help groups.
- Behavioral therapy.
- Rehab facilities.
- Alcoholics Anonymous.
Understanding wet brain syndrome: causes, symptoms, and treatment
Wet brain is a debilitating neurological syndrome affecting those with severe thiamine deficiency, particularly those struggling with alcohol addiction. It can lead to memory problems, confusion, and difficulty with muscle coordination - and if it develops into Korsakoff’s psychosis, the symptoms are permanent.
Make sure to spot any signs of wet brain syndrome as soon as possible and speak to your healthcare provider for the necessary information to reverse the symptoms of this illness.
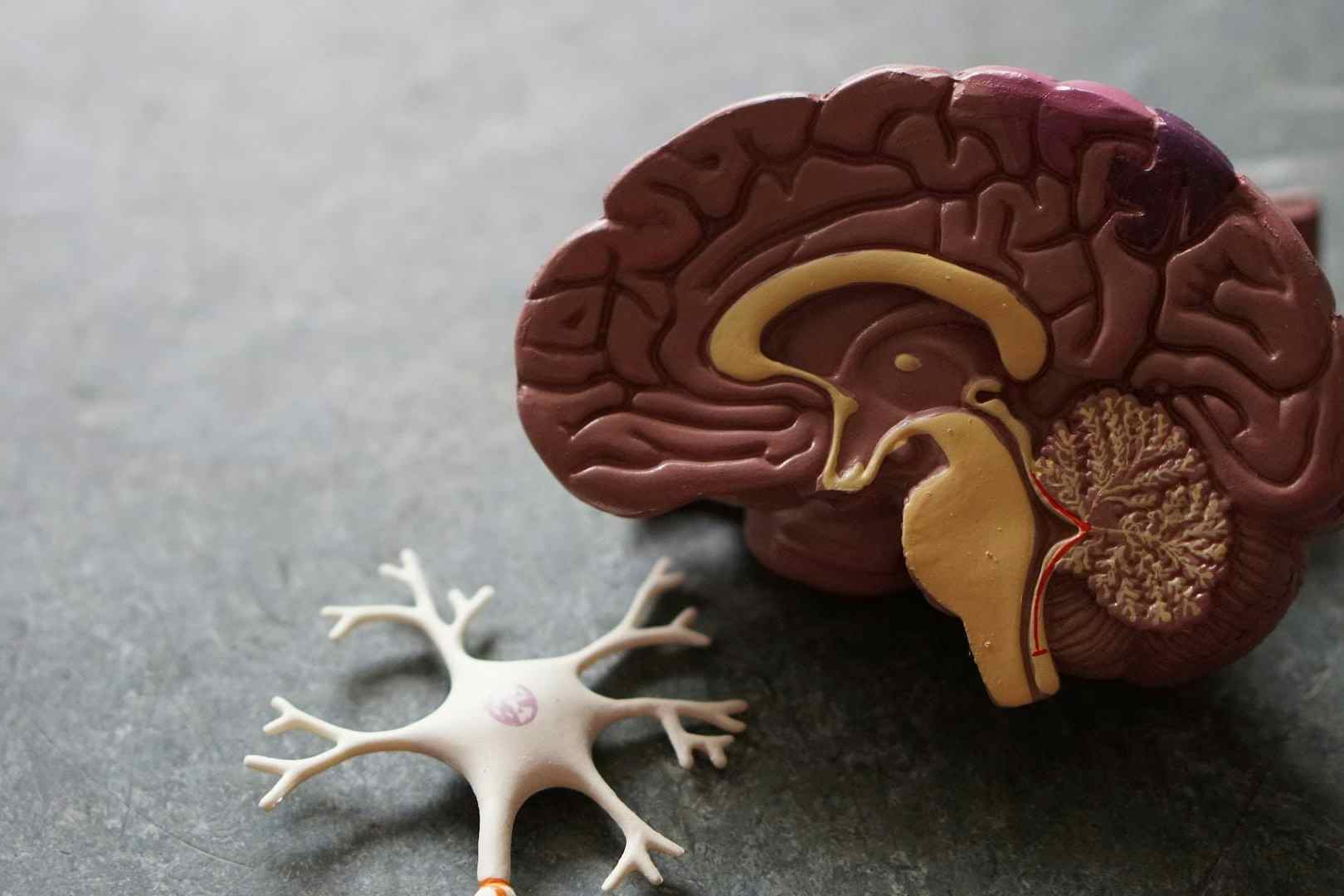
Image Credit: Robin Weermeijer at Unsplash